Have you ever wondered why after a night of drinking some alcoholic beverages followed by a raid of the pantry you feel a little blue or slightly anxious? Maybe you’ve had an upset stomach before a big test or meeting? Did you notice a positive shift in depression or anxiety when you started focusing on your nutrition?
Science will tell you that you are not alone! Gut health has been studied for hundreds of years but modern research is providing evidence of a direct correlation with mental health.
So first, what are we really talking about when we say “gut health?”
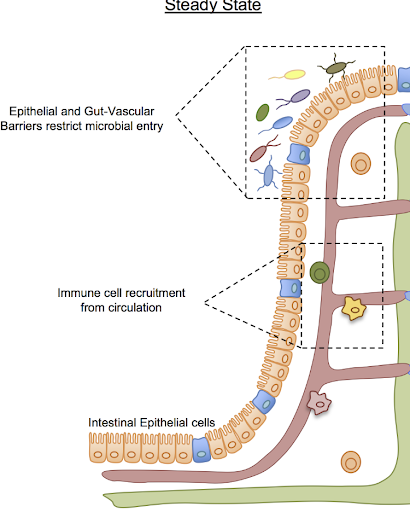
We are really looking at two different aspects. First, is the barrier that separates you from your poo (you know you love these sweet rhymes) intact? Meaning, do you have any disruption to your intestinal barrier?
Secondly, is the composition of your “microbiome” associated with health or disease?
To go a little further, each person has trillions of microbes that live within their body. The totality of these microbes within us makes up our gut microbiota. Our gut microbiota is formed partly from our mother during birth and from interactions with our environment thereafter. What’s interesting is that healthy people tend to have a very distinct “set” of bacteria from people that experience chronic disease.
Gut health and an individual’s own microbiome can be linked to immunity, disease, behavior, mood, and much more, but for the purpose of this blog, we will only be examining its effect on anxiety and depression. 0
Antidepressants and The Gut
To be very clear, this next section is designed to help establish a connection between the gut and the brain. It is not a “knock” on antidepressants, nor is it a call to come off medication. If you have questions, please contact your doctor directly.
Antidepressants, also commonly used to treat anxiety and other mood disorders, are known to affect not only brain chemistry, but also the gut because of their antimicrobial properties. 1 The most commonly prescribed antidepressants are SSRIs (selective serotonin reuptake inhibitors). Serotonin is often thought of as the “happy” hormone. While some serotonin is produced in the brain, the majority of it is produced in the gut. 2 Serotonin is understood to help regulate mood and behavior, hunger levels and digestion, sleep, memory, as well as sexual desire and function. 3
Many people experience weight gain as a side effect of antidepressants. Studies suggest the link between antidepressants and weight gain is caused by the medication’s ability to block multiple receptors in the body. 4 While the full extent of serotonin’s role in appetite and metabolism is not completely understood, switching from one subtype of SSRI to another might be enough to curb the symptom of weight gain. The caveat to this being that different SSRIs affect different receptors and could be less effective in treating the mood disorder in the individual. 5
Let's look at some studies:
Scientists have used “germ-free” mice (which completely lack bacteria in their gut) to observe behavioral and emotional responses to lack of microbiota as well as specific strains of microbes. Mice that were born into sterile environments, with no exposure to bacteria, had higher levels of anxiety and depression-like behavior than mice who were not. These “Germ-free” mice were shown to have decreased levels of serotonin receptors known as 5-HT. 6 Another study on GF mice found that they produced around 60% less serotonin than their counterparts. 7 Together this begins to inform us that there may be a symbiotic relationship between our gut bacteria and the body’s ability to produce the appropriate amount of this critical neurotransmitter.
Looking a little deeper…
- Its well known that different strains of mice have different levels of anxiety… and interestingly this correlates with different bacteria in their guts. To test whether this could be a “causative” relationship (instead of just correlating) scientists transferred bacteria from stress prone mice into regular mice. What was amazing was that these mice quickly began to exhibit anxiety ridden behavior. Alternatively, they transferred bacteria from “normal” mice, whose bacteria had not been altered, into the stress prone mice and observed that their behavior normalized. This provides strong evidence that the type of bacteria in your gut can be a DRIVER anxiety and stress 8
- When physically restrained for a short duration, Germ free mice released more stress hormones than mice with microbiomes. When given a probiotic strain of bacteria (Bifidobacterium infantis) the originally GF mice exhibited normal levels of stress hormones in the same situation. 9 This begins to teach us that Bifidobacterium bacteria may be helpful in preventing excessive anxiety or stress. Interestingly, Bifido is one of the first bacteria transferred to newborn babies through breast milk
When we start to look at studies in humans, we note similar connections.
- A three week study on healthy individuals ingesting a probiotic drink found that the previously depressed noted themselves to be happier after consumption. Those that noted they were happy prior to the study did not see any change in mood. 10
- A study of Dutch infants found that mothers who were stressed during pregnancy gave birth to children whose gut makeup was more prone to inflammation. Children whose mothers reported high stress levels during pregnancy had significantly higher levels of certain bacteria known to be pathogenic and lower levels of beneficial bacteria. The infants were also more likely to have gastrointestinal issues and allergies. 11
- A study on chimps found that mothers who were startled with loud noises gave birth to chimps with fewer “healthy” bacteria (lactobacilli) in their gut than their counterparts. The same bacteria (lactobacilli) was noticeably diminished in stressed students during exam weeks as opposed to the beginning of the semester. 12
Overall, we can conclude that there’s strong correlative evidence, and some causative evidence in animals, that the type of bacteria that reside in our guts can influence our mood, either directly or indirectly through the immune system. This whole world of research is rather new, but scientists are becoming more and more interested in it daily. We know that bacteria and our immune system are intimately connected. We know that the immune system and our nervous system (which controls mood) are intimately connected. Now we just have to figure out how all the pieces work together.
So knowing this, how can we improve our own gut health to try and impact our mood?
(Again, this is NOT meant to be a replacement for prescribed medicine, but instead an additional approach that can be considered with your health care professional.)
The first key is understanding that we all have a unique makeup of gut microbiota and that what works for one will not work for all.
The second key is noting the two-way path that is the brain-gut axis. If you take all the right steps to promote a healthy gut but live in a world of physical and emotional stress, you are not inciting real change.
Some simple ways to promote a healthy gut:
- Eat a diverse selection of fruits and veggies (these also tend to be prebiotics which benefit the gut). Fiber is not digested by the gut but rather the bacteria in the gut. Fiber promotes the growth of healthy bacteria and helps curb the growth of disease promoting bacteria. 13
- Eat cruciferous vegetables like broccoli, cauliflower, and cabbage. Regular consumption of these foods promotes positive changes in the gut bacteria. 14
- Eat fermented foods. Fermented foods like sauerkraut, kimchi, kombucha, pickled foods, and yogurt have already been modified by microbes. They also tend to be rich in lactobacilli, a healthy bacteria. 15
- Avoid artificial sweeteners as they are thought to negatively modify the microbiota. 16
- Consider a probiotic. While taking a probiotic will not permanently change the microbiota, it is shown to benefit gut health in the presence of some disease. 17 We typically recommend PRO-15 by hyperbiotics.
- Minimize stress. Create habits that allow you to relax and unwind and put them into practice each and every day.
We're learning more everyday about how important gut health is for nearly all aspects of our health and fitness. If you're interested in exploring ways to change your diet and lifestyle to maximize your gut health, reach out to us here or check out our coaching options.





